Building Strong Bones
Osteoporosis, often referred to as the “silent disease,” is a condition characterized by fragile bones, making them more prone to fractures. While it’s mostly affects older adults, especially women after menopause, the steps you take in your younger years significantly impact your bone health later in life. Here’s a comprehensive guide on how to prevent osteoporosis through lifestyle choices, diet, and exercise.
Understanding Osteoporosis:
Osteoporosis, or “bones with holes,” occurs when bones lose minerals like calcium faster than they’re replaced, resulting in reduced density, weakened strength, and increased susceptibility to fractures. Often, individuals remain unaware of their condition until a fracture occurs, highlighting the importance of investigating risk factors that affect bone health. Early detection and intervention are crucial in preventing unwanted fractures, as osteoporosis typically presents no noticeable signs or symptoms. Medical treatment can mitigate further bone loss and lower fracture risk, while lifestyle adjustments play a key role in supporting overall bone health.
Diagnosis
The most dependable method for diagnosing osteoporosis involves measuring bone density through a dual-energy absorptiometry scan (DXA). This painless procedure assesses bone density, typically at the hip, spine, and occasionally the forearm.
You can qualify for a Medicare rebate for a DXA scan if you:
*Previously diagnosed with osteoporosis
*Experienced one or more osteoporosis-related fractures
*Age 70 or older
*Living with chronic conditions such as rheumatoid arthritis, coeliac disease, or liver disease
*Long-term use of corticosteroids
Your doctor can determine if you meet the requirements for a Medicare rebate. Even if you don’t qualify for the rebate but have risk factors needing assessment, you may still undergo a DXA scan, albeit incurring an out-of-pocket expense.
Risk Factors
Several risk factors contribute to osteoporosis, including some unchangeable ones like being female or having a close relative with a history of osteoporotic fractures.
More factors that increase risk are:
*Not enough calcium in your diet
*Low levels of vitamin D
*Smoking or drinking too much alcohol
*Not being physically active
*Menopause before age 45
*Losing periods due to low oestrogen
Certain medical conditions and medications can increase the risk of osteoporosis. These include:
*Early onset of menopause or low testosterone levels
*Thyroid disorder or hyperthyroidism
*Rheumatoid arthritis
*Chronic liver and kidney ailments
*Conditions impacting nutrient absorption such as Crohn’s disease, celiac disease, and other inflammatory bowel conditions
*Prolonged use of medications like corticosteroids for rheumatoid arthritis, asthma, and other illnesses
*Certain therapies for prostate cancer and breast cancer
Prevention
1. Adopt a Balanced Diet:
-Ensure your diet includes calcium-rich foods like dairy products, leafy greens, and fortified foods.
-Consume an adequate amount of vitamin D, which helps your body absorb calcium. Sun exposure and fortified foods are excellent sources.
-Limit caffeine and alcohol intake, as they can interfere with calcium absorption.
2. Prioritize Physical Activity:
-Engage in weight-bearing exercises like walking, jogging, dancing, and strength training to stimulate bone growth.
-Incorporate balance and flexibility exercises to reduce the risk of falls and fractures.
3. Avoid Smoking and Excessive Alcohol Consumption:
-Smoking can significantly decrease bone density and increase the risk of fractures.
-Limit alcohol intake, as excessive consumption can weaken bones and increase the risk of falls.
4. Maintain a Healthy Body Weight:
-Being underweight increases the risk of bone loss and fractures. Aim for a healthy weight through a balanced diet and regular exercise.
5. Assess Your Risk Factors:
-Understand your family history and personal risk factors for osteoporosis.
-Talk to your healthcare provider about bone density testing, especially if you’re postmenopausal or have other risk factors.
6. Ensure Safe Home Environments:
-Reduce the risk of falls by removing tripping hazards, installing grab bars in bathrooms, and improving lighting in your home.
7. Stay Informed and Proactive:
-Educate yourself about osteoporosis and its risk factors.
-Schedule regular check-ups with your healthcare provider to monitor your bone health and discuss preventive measures.
8. Get Durable Back brace:
–TLSO (thoracic-lumbo-sacral orthosis) back brace is recommended to immobilize the spine and minimize the risk of bone fractures.
-It also reduces back pain by limiting motion and easing the stiffness associated with osteoporosis.
Conclusion:
Preventing osteoporosis is an ongoing process that requires a combination of healthy lifestyle choices, dietary habits, and regular exercise. By adopting these preventive measures early on, you can significantly reduce your risk of developing osteoporosis and enjoy strong, healthy bones well into old age. Remember, it’s never too early or too late to start prioritizing your bone health.
How can Daphco help you with your Osteoporosis?
At Daphco Medical Equipment, we provide a range of back braces designed to support your spine and prevent curvature, reducing the risk of osteoporosis. If you’re covered by Medicare, simply fill out our contact form, and we’ll reach out to discuss how you can obtain the brace through your insurance.
Search Articles
Latest Articles
28th Feb, 24
23rd Feb, 24
20th Feb, 24
15th Feb, 24
13th Feb, 24
 888-616-4156
888-616-4156 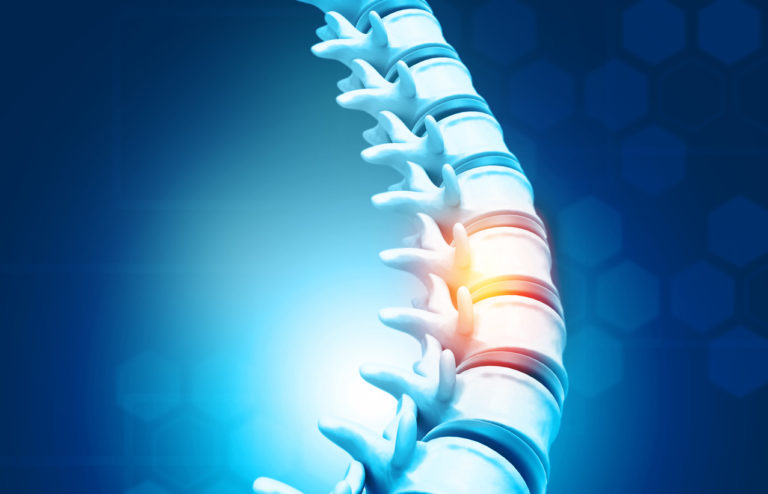





 28th Feb, 24
28th Feb, 24